Items filtered by date: December 2017
Symptoms and Effective Treatment for Sever’s Disease
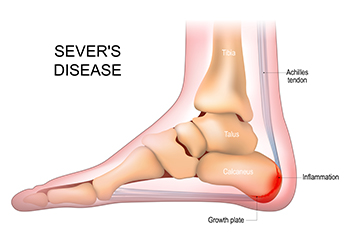
Sever's disease, also known as calcaneal apophysitis, is a common but often misunderstood condition affecting children and adolescents, especially those active in sports. It is not a traditional disease but rather a painful growth plate disorder. Understanding its symptoms and appropriate treatment is vital for parents and young athletes. The hallmark symptom of Sever's disease is heel pain, typically at the back or along the bottom of the heel. Pain tends to worsen during or after physical activities and may cause limping or discomfort when walking or running. The condition arises when the growth plate at the back of the heel bone becomes inflamed due to repetitive stress. Fortunately, Sever's disease is treatable. Getting adequate rest and taking over-the-counter pain relievers can help alleviate discomfort. Stretching exercises and may also be recommended to improve flexibility, and strengthen the calf muscles. Wearing supportive footwear with cushioned insoles may help reduce heel pressure. By recognizing the symptoms and seeking appropriate treatment, parents and young athletes can manage Sever's disease effectively, allowing for a smoother path to recovery and a return to their favorite activities. If your active child has heel pain, it is strongly suggested that you consult a podiatrist who can accurately diagnose and treat Sever’s disease.
Sever's disease often occurs in children and teens. If your child is experiencing foot or ankle pain, see Dr. Ronald Sheppard from Warren-Watchung Podiatry Center. Our doctor can treat your child’s foot and ankle needs.
Sever’s Disease
Sever’s disease is also known as calcaneal apophysitis, which is a medical condition that causes heel pain I none or both feet. The disease is known to affect children between the ages of 8 and 14.
Sever’s disease occurs when part of the child’s heel known as the growth plate (calcaneal epiphysis) is attached to the Achilles tendon. This area can suffer injury when the muscles and tendons of the growing foot do not keep pace with bone growth. Therefore, the constant pain which one experiences at the back of the heel will make the child unable to put any weight on the heel. The child is then forced to walk on their toes.
Symptoms
Acute pain – Pain associated with Sever’s disease is usually felt in the heel when the child engages in physical activity such as walking, jumping and or running.
Highly active – Children who are very active are among the most susceptible in experiencing Sever’s disease, because of the stress and tension placed on their feet.
If you have any questions, please feel free to contact one of our offices located in Marlboro and Watchung, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle injuries.
Heel Pain
Have you ever gotten up from a chair or out of bed in the morning, and upon taking that first step, feel like your heel has stepped on a tack? Many people experience a feeling of sharp pain which radiates into their arch from their heel and which does not allow them to put their heel on the floor. Sometimes they need to sit back down, stand only on their toes and use the wall for balance. If you can take a few steps, it seems to go away and lessen, allowing you to then resume your activity. Later, throughout your day and after a period of rest, it can happen again. If this sounds familiar you may be suffering from your first attack of heel pain.
Heel pain is a debilitating condition that affects day to day activities. Running and walking both causes stress on the heel because the heel is the part of the foot that hits the ground first. This means that the heel is taking on your entire weight. Diagnosis and treatments for heel pain can be easily found through your podiatrist.
Plantar Fasciitis
One of the main causes of heel pain is a condition known as plantar fasciitis. The plantar fascia is a band of tissue that extends along the bottom of the foot, from the toe to the bottom of the heel. A rip or tear in this ligament can cause inflammation of these tissues, resulting in heel pain. People who do not wear proper fitting shoes are often at risk of developing problems such as plantar fasciitis. Unnecessary stress from ill-fitting shoes, weight change, excessive running, and wearing non-supportive shoes on hard surfaces are all causes of plantar fasciitis.
Achilles Tendonitis
Achilles tendonitis is another cause of heel pain. Similar to plantar fasciitis, inflammation of the Achilles tendon will cause heel pain due to stress fractures and muscle tearing. A lack of flexibility of the ankle and heel is an indicator of Achilles tendonitis. If left untreated, this condition can lead to plantar fasciitis and cause even more pain on your heel.
Heel Spur
A third cause of heel pain is a heel spur. A heel spur occurs when the tissues of the plantar fascia undergo a great deal of stress, leading to a separation of the ligament from the heel bone entirely. This results in a pointed fragment of bone on the ball of the foot, known as a heel spur.
Heel Pain Caused by Bursitis

Heel pain can be debilitating, and one common cause is bursitis. This condition occurs when the bursa, a small fluid-filled sac that cushions and lubricates the joints, becomes inflamed. In the case of heel bursitis, the bursa located at the back of the heel becomes irritated and swollen. The bursa is typically aggravated by activities that put pressure on the affected area, such as walking or wearing tight shoes. Inflammation can also be caused by repetitive overuse or direct trauma to the heel. Diagnosis usually involves a physical examination, and sometimes imaging tests like X-rays or ultrasound are used to rule out other conditions. Treatment options range from rest and ice to reduce inflammation, to physical therapy and orthotic shoe inserts for support. In some cases, a podiatrist may recommend corticosteroid injections to alleviate pain and inflammation. If you're experiencing persistent heel pain, it is suggested that you consult a podiatrist for a proper diagnosis and personalized treatment plan. With the right care, heel bursitis can be managed effectively, allowing you to get back on your feet pain-free.
Many people suffer from bouts of heel pain. For more information, contact Dr. Ronald Sheppard of Warren-Watchung Podiatry Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact one of our offices located in Marlboro and Watchung, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Gout Pain Can Be Managed
Bunions
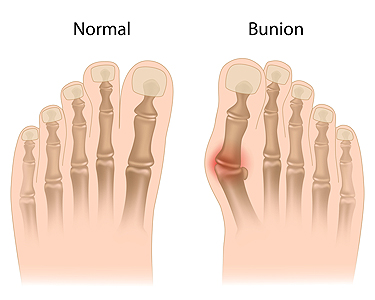
A bunion is a bump that forms at the base of the big toe. Bunions form when the big toe pushes against the next toe, which forces the big toe joint to get bigger and stick out. As a result, the skin over the bunion may start to appear red and it may feel sore.
There are risk factors that can increase your chances of developing bunions. People who wear high heels or ill-fitting shoes are more likely to develop them, in addition to those who have a genetic history of bunions or have rheumatoid arthritis.
The most obvious way to tell if you have a bunion is to look for the big toe pushing up against the toe next to it. Bunions produce a large protrusion at the base of the big toe and may or may not cause pain. Other symptoms are redness, swelling, and restricted movement of the big toe if you have arthritis.
Nonsurgical methods are frequently used to treat bunions that aren’t severe. Some methods of nonsurgical treatment are orthotics, icing and resting the foot, taping the foot, and pain medication. Surgery is usually only required in extreme cases. However, if surgery is needed, some procedures may involve removing the swollen tissue from around the big toe joint, straightening the big toe by removing part of the bone, or joining the bones of your affected joint permanently.
Your podiatrist will diagnose your bunion by doing a thorough examination of your foot. He or she may also conduct an x-ray to determine the cause of the bunion and its severity.
Treatment Options for Bunions
Bunions are painful bumps at the base of the big toe that can make walking uncomfortable and even interfere with your daily activities. When it comes to non-surgical treatment of bunions, often the first step is changing your footwear. Shoes with a wider toe box can give your toes more room to breathe and reduce friction. Toe spreaders can also be beneficial by helping to maintain proper toe alignment and preventing further deviation. Finally, your podiatrist can prescribe anti-inflammatory drugs or pain relievers to provide relief. If non-surgical options fail to provide relief and the bunion severely impacts your daily life, bunion surgery is an option to consider. Two common types of bunion surgery are osteotomy and fusion. Osteotomy involves removing a portion of the bone to realign the toes properly. Fusion surgery entails joining the joint at the base of the toe and is typically reserved for more severe cases. Recovery from bunion surgery can take up to eight weeks, while swelling may persist for several months. A podiatrist can provide personalized advice based on the severity of your condition and your individual needs. It is suggested that you make an appointment today.
If you are suffering from bunion pain, contact Dr. Ronald Sheppard of Warren-Watchung Podiatry Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact one of our offices located in Marlboro and Watchung, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
All About Plantar Warts
Plantar warts are warts that are only found on the feet, hence the term “plantar”, which means “relating to the foot.” They are caused by the human papillomavirus, or HPV, and occur when this virus gets into open wounds on the feet. The warts themselves are hard bumps on the foot. They are easily recognizable, mostly found on the heels or ball of the foot. Plantar warts are non-malignant, but they can cause some pain, discomfort, and are often unsightly. Removing them is a common step toward treating them.
Plantar warts can cause some pain while standing, sometimes felt as tenderness on the sole of your foot. Unless the wart has grown into the foot behind a callus, you will be able to see the fleshy wart. A podiatrist should only be consulted if there is an excessive amount of pain. Plantar warts are not cancerous or dangerous, but they can affect your walking and continually reappear. Anyone who suffers from diabetes or a compromised immune system disease should seek out care immediately.
Podiatrists are easily able to diagnose plantar warts. They usually scrape off a tiny bit of the rough skin to make tiny blood clots visible and examine the inside of warts. However, a biopsy can be done if the doctor is not able to diagnose them from simply looking at them. Although plantar warts usually do not require an excessive amount of treatment, there are ways to go about removing them. A common method is to freeze them off using liquid nitrogen, removing them using an electrical tool, or burning them off via laser treatment. For a less invasive treatment option, topical creams can be used through a doctor’s prescription. This treatment method takes more time, however. Keep the wart covered for protection in between daily treatments.
The best way to avoid developing plantar warts is to avoid walking barefoot in public places. Avoid this especially if you have open sores or cuts on your feet. It is also important to avoid direct contact with warts in general, as they are highly contagious.
Treatment for Plantar Warts

A plantar wart, which is a growth on the sole of your foot, is caused by exposure to the human papillomavirus, or HPV. Although this type of infection is more common among children and young adults, it can affect anyone. You might wonder how you end up with this unwelcome visitor. It's simple, the infection is caused by direct contact with the virus through a break in your skin. Sometimes, it can take months after exposure for a plantar wart to appear. The wart often starts as a small, rough patch on your foot's sole but can expand over time. These growths disrupt the usual skin lines on your feet and might display tiny black dots due to clogged blood vessels. Treatment options vary based on how the warts bother you. Salicylic acid treatments may or may not be effective. More advanced treatment includes the application of liquid nitrogen to freeze the skin, though this process can cause discomfort and may take several applications. If you think you may have a plantar wart, especially if it becomes painful or shows signs of infection, it is suggested that you make an appointment with a podiatrist. This qualified foot doctor can evaluate the problem and suggest a proper course of treatment.
Plantar warts can be very uncomfortable. If you need your feet checked, contact Dr. Ronald Sheppard from Warren-Watchung Podiatry Center. Our doctor will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact one of our offices located in Marlboro and Watchung, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What is a Podiatrist?
The branch of medicine that is focused on the treatment, diagnosis, and study of disorders of the lower leg, ankle and foot is referred to as podiatry. Because people often spend a great deal of their time on their feet, many problems in this area can occur. A person seeks help from the field of podiatry when they need treatment for heel spurs, bunions, arch problems, deformities, ingrown toenails, corns, foot and ankle problems, infections, and problems with the foot that are related to diabetes and additional diseases.
To treat problems of the foot, ankle or lower leg, a podiatrist may prescribe physical therapy, drugs, perform surgery, or set fractures. Individuals may also be recommended to wear corrective shoe inserts, custom-made shoes, plaster casts and strappings in order to correct deformities.
When trying to gather information on a patient problem, a scanner or force plate may be used in order to design orthotics. During this procedure, patients are told to walk across a plate that is connected to a computer; the computer then takes a scan of the foot and indicates weight distribution and pressure points. The computer readouts will give the podiatrist information to help them determine the correct treatment plans.
Diagnosis is also provided through laboratory tests and x-rays. Through the foot, the first signs of serious problems such as heart disease, diabetes and arthritis can show up. For example, individuals that have diabetes may frequently have problems such as infections and foot ulcers because they experience poor circulation in the foot area. A podiatrist can then have consultations with patients when symptoms arise. Referrals will then be made to specialists that handle the greater health problems.
Some podiatrists have their own independent, private practices or clinics where they have a small staff and administrative personnel. Many podiatrists work within group practices. They usually spend time performing surgery in ambulatory surgical centers or hospitals, or visit patients in nursing homes. Podiatrists typically spend between 30 to 60 hours of week working. Some podiatrists specialize in public health, orthopedics, surgery, or primary care. Other fields include specialties in geriatrics, dermatology, pediatrics, diabetic foot care and sports medicine.
Some podiatrist specialists complete extra training in the area of foot and ankle reconstruction that results from the effects of physical trauma or diabetes. There are also surgeons that perform surgery of a cosmetic nature to correct bunions and hammertoes.
What Is a Podiatrist's Job Description?

Podiatrists are medical professionals who play a vital role in foot and ankle health. Their primary focus is diagnosing, treating, and preventing various conditions related to the foot and ankle. From routine checkups to complex surgeries, a podiatrist’s responsibilities encompass a variety of tasks. Podiatrists assess patients' foot and ankle health, conduct thorough examinations, and utilize diagnostic tools to identify issues. They provide personalized treatment plans, including medication, physical therapy, orthotics, and surgical interventions when necessary. As experts in their field, podiatrists are dedicated to ensuring optimal foot health and aiding patients in maintaining mobility, comfort, and overall well-being. If you are interested in pursuing the field of podiatry as a profession, it is suggested that you speak with this type of doctor who can help you make an informed decision about this career choice.
If you are experiencing pain in the feet or ankles, don’t join the stubborn majority refusing treatment. Feel free to contact Dr. Ronald Sheppard from Warren-Watchung Podiatry Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Podiatrist?
Someone would seek the care of a podiatrist if they have suffered a foot injury or have common foot ailments such as heal spurs, bunions, arch problems, deformities, ingrown toenails, corns, foot and ankle problems, etc.
Podiatric Treatment
A podiatrist will treat the problematic areas of the feet, ankle or lower leg by prescribing the following:
- Physical therapy
- Drugs
- Orthotic inserts or soles
- Surgery on lower extremity fractures
A common podiatric procedure a podiatrist will use is a scanner or force plate which will allow the podiatrist to know the designs of orthotics. Patients are then told to follow a series of tasks to complete the treatment. The computer will scan the foot a see which areas show weight distribution and pressure points. The podiatrist will read the analysis and then determine which treatment plans are available.
If you have any questions please feel free to contact one of our offices located in Marlboro and Watchung, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.